If you have ever felt self-conscious about darker skin around your intimate areas — the bikini line, inner thighs, groin, or vulvar region — you are definitely not alone. This is one of the most common yet least talked-about skincare concerns, especially among women in India.
Intimate area lightening is something millions of people quietly research online. But here is the problem: most of the information out there is either outdated, dangerously wrong, or just plain misleading. Some blogs tell you to rub lemon juice on your most sensitive skin. Others push harsh bleaching creams that can permanently damage delicate tissue.
This article is different. It is built entirely on dermatology-backed information, real ingredient science, and safety-first guidance. By the end, you will know exactly which methods are safe, which ones to stay far away from, and how to build a simple routine that actually delivers results — without harming your body.
Why Does Intimate Area Darkening Happen? (And Why It Is Totally Normal)
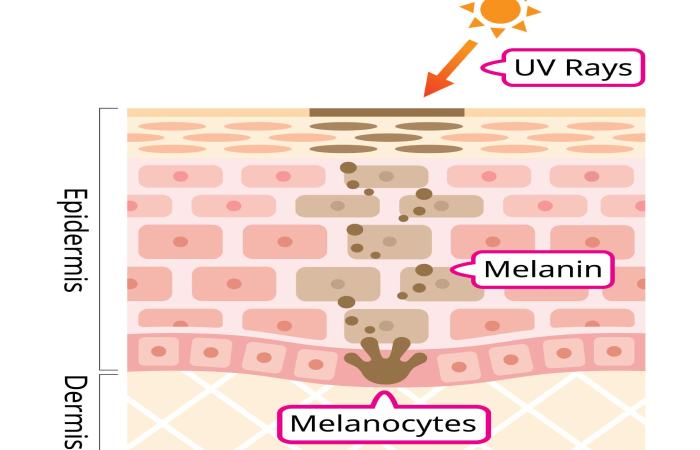
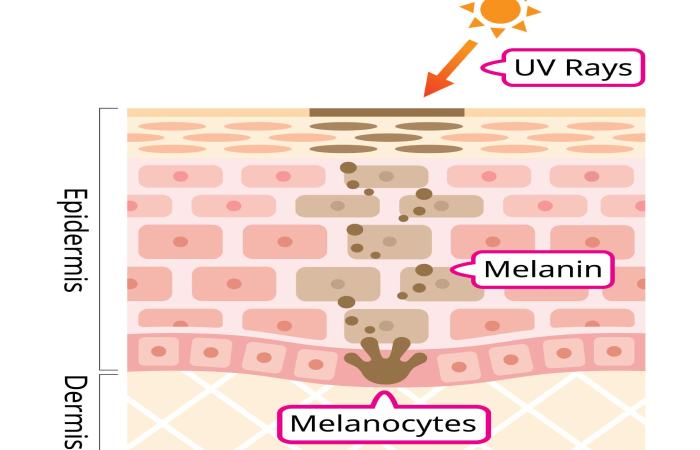
Before jumping into solutions, it helps to understand the root cause. Darker skin in intimate areas is medically called hyperpigmentation, and it happens because of an increase in melanin — the natural pigment your skin produces.
This is not a sign of poor hygiene, disease, or anything alarming. It is a biological response. Dermatologists consistently confirm that why private areas darken is one of the most normal skin changes that happens after puberty. Here are the most common reasons it happens:
Hormonal shifts are the number one trigger. Estrogen and progesterone levels change significantly during pregnancy, after childbirth, during menopause, and when using hormonal contraceptives like pills or IUDs. These hormonal fluctuations directly stimulate melanocytes (the cells that make melanin) to produce more pigment.
Friction and irritation play a huge role too. Tight jeans, synthetic underwear, shaving, waxing, and even daily walking or exercise create constant low-grade friction in the groin and bikini area. Over time, this irritation triggers the skin’s protective response — more melanin production.
Genetics also matter. People with naturally deeper skin tones tend to have more melanin activity everywhere, including intimate zones. This is completely normal and not something that needs “fixing” unless you personally want to even out your tone.
Aging contributes as well. As skin thins and loses elasticity with age, existing pigment becomes more visible and concentrated.
A Quick Reality Check
| Factor |
How It Causes Darkening |
| Hormonal changes (pregnancy, menopause, birth control) |
Directly stimulates melanin production |
| Friction (tight clothes, shaving, walking) |
Triggers skin’s protective pigment response |
| Genetics |
Higher baseline melanin in skin folds |
| Aging |
Thinner skin makes pigment more visible |
| Harsh soaps or products |
Causes inflammation, which worsens pigmentation |
| Certain medications |
Some drugs increase photosensitivity or melanin activity |
Who Should Read This — And Who Should See a Doctor First
This guide is written for anyone who has noticed gradual, even darkening in their intimate areas and wants to lighten it safely at home or with gentle professional help.
This is NOT for you if:
- The darkening appeared suddenly or very recently without an obvious cause
- You have unusual redness, pain, discharge, or itching alongside the darkening
- You suspect an infection, hormonal disorder like PCOS, or any underlying health condition
- You are pregnant or breastfeeding and want to start a new skincare treatment
In any of these cases, please see a dermatologist or gynaecologist first. Sudden changes in skin pigmentation can sometimes signal something that needs medical attention — and no blog article should replace a professional opinion.
The Ingredients That Actually Work (Science-Backed)
Here is where things get interesting. Not all “lightening” ingredients are created equal — and many of the ones marketed aggressively in India are actually the ones you should avoid on sensitive skin. Let’s break down the ones that dermatologists genuinely trust for intimate areas.
Alpha Arbutin — The Gentlest Brightener
Alpha arbutin is derived from bearberry, cranberry, or mulberry leaves. It works by slowly releasing a tiny amount of hydroquinone into the skin — but in such a controlled way that it does not cause the irritation or rebound darkening that pure hydroquinone can.
It inhibits tyrosinase, the enzyme responsible for melanin production. Because it works gradually, it is considered one of the safest options for sensitive skin areas. Peer-reviewed research on arbutin’s depigmenting mechanism published on NCBI confirms that alpha arbutin is significantly more effective than regular arbutin at inhibiting human tyrosinase. Dermatologists often recommend concentrations of 1–2% for intimate use.
Why it works well for Indian skin: Alpha arbutin does not cause rebound hyperpigmentation (a risk with stronger agents), making it particularly suitable for melanin-rich skin tones common across India.
Kojic Acid — A Powerful but Gentle Tyrosinase Inhibitor
Kojic acid is a naturally occurring compound derived from fungi — the same fermentation process used to make sake and soy sauce. Research published in the International Journal of Research in Dermatology (2025) confirms it works comparably to hydroquinone for reducing pigmentation, but with significantly fewer side effects.
It blocks the copper ions that tyrosinase needs to function. Without functional tyrosinase, your skin simply cannot produce as much melanin. WebMD’s dermatology team breaks down how kojic acid inhibits melanin in a way that makes the science easy to follow.
Ideal concentration for intimate areas: 1–2%. Anything higher may cause irritation on delicate skin.
Niacinamide (Vitamin B3) — The Multi-Tasking Soother
Niacinamide works differently from the other two. Rather than stopping melanin production, it reduces melanin transfer — meaning your skin still makes melanin, but less of it reaches the surface where you can see it.
A study referenced in the British Journal of Dermatology found that 4% niacinamide significantly reduced hyperpigmentation after just 8 weeks. More recent research has shown 5% niacinamide can perform comparably to 4% hydroquinone — but with far better tolerability and no long-term risks.
Niacinamide is also anti-inflammatory, which is a huge bonus for intimate areas where irritation is already common. It soothes, hydrates, and brightens all at the same time.
Vitamin C (L-Ascorbic Acid or Ascorbyl Glucoside)
Vitamin C is a potent antioxidant that fights hyperpigmentation through multiple pathways: it inhibits melanin synthesis, neutralizes free radicals that worsen pigmentation, and boosts collagen production for smoother skin.
For intimate areas specifically, ascorbyl glucoside is a better choice than L-ascorbic acid because it is more stable and less likely to irritate sensitive skin.
Licorice Root Extract
This plant extract — available in many Ayurvedic and modern skincare products sold across India — contains glabridin, a compound that inhibits tyrosinase without irritation. It is anti-inflammatory and gentle enough for sensitive zones.
How These Ingredients Compare
| Ingredient |
How It Works |
Best Concentration for Intimate Areas |
Irritation Risk |
Time to See Results |
| Alpha Arbutin |
Slowly releases hydroquinone to inhibit tyrosinase |
1–2% |
Very Low |
4–8 weeks |
| Kojic Acid |
Blocks copper ions needed by tyrosinase |
1–2% |
Low |
4–8 weeks |
| Niacinamide |
Reduces melanin transfer to skin surface |
4–5% |
Very Low |
6–8 weeks |
| Vitamin C (Ascorbyl Glucoside) |
Antioxidant; inhibits melanin synthesis |
5–10% |
Low |
4–6 weeks |
| Licorice Root Extract |
Glabridin inhibits tyrosinase |
As per product label |
Very Low |
6–10 weeks |
The 5 Biggest Mistakes People Make (And How to Avoid Them)
Based on the most common questions and concerns in this space, here are the errors that hold people back — or actively harm their skin.
Mistake 1: Using Lemon Juice Directly on Intimate Skin
Lemon juice is highly acidic (pH around 2). While it does contain vitamin C, applying it undiluted to the delicate skin of intimate areas is a recipe for chemical burns, inflammation, and — ironically — worse pigmentation from the resulting irritation.
What to do instead: Use a properly formulated vitamin C product designed for sensitive skin.
Mistake 2: Grabbing Any “Fairness Cream” Off the Shelf
Many over-the-counter fairness creams in India contain high concentrations of hydroquinone, mercury, or corticosteroids. These are not safe for intimate areas. Hydroquinone above 2% can thin the skin. Mercury is toxic. Corticosteroids used without medical guidance increase the risk of fungal infections in already moisture-rich zones.
What to do instead: Look for products specifically formulated for intimate or sensitive skin. Check the ingredient list. If you see hydroquinone above 2%, mercury, or unnamed “fragrance,” put it back.
Mistake 3: Being Impatient and Doubling Up on Products
Skin lightening in intimate areas is a slow, gentle process. Applying two or three products at once, or using them more frequently than directed, does not speed things up — it causes irritation, which triggers more melanin and makes darkening worse.
What to do instead: Start with one product. Use it consistently for 4–6 weeks before deciding if it is working.
Mistake 4: Skipping Moisturizer
Dry, irritated skin is significantly more prone to darkening. Many people focus entirely on the “lightening” step and ignore hydration completely. This creates a cycle: dry skin → irritation → more pigment → disappointment.
What to do instead: Always apply a fragrance-free, gentle moisturizer after any treatment. Look for ingredients like glycerin, hyaluronic acid, or aloe vera.
Mistake 5: Using Regular Body Soap
Standard body soaps have a pH that is too alkaline for the intimate area. They strip the skin’s natural oils and disrupt the delicate pH balance, leading to chronic low-grade irritation.
What to do instead: Use a pH-balanced, fragrance-free intimate wash. Many Ayurvedic brands in India offer gentle options.
Myths vs. Facts: Let’s Clear the Air
| Myth |
Fact |
| “Dark intimate areas mean poor hygiene” |
Darkening is caused by hormones, friction, and genetics — not cleanliness |
| “Bleaching creams work faster, so they’re better” |
Harsh bleaching creams cause more harm than good on sensitive skin. Gentle, sustained brightening is always safer |
| “This problem only affects women” |
Men also experience darkening in the groin, inner thighs, and underarm areas |
| “If it stings, it’s working” |
Stinging or burning is a warning sign of irritation — stop immediately |
| “You only need to do this once” |
Pigmentation, especially hormonal, can return. Maintenance and prevention are ongoing |
| “Turmeric paste will lighten skin instantly” |
Turmeric has anti-inflammatory properties, but it does not meaningfully lighten pigmentation on its own |
Your Step-by-Step Safe Lightening Routine
Here is a simple, practical routine you can follow at home. It uses widely available ingredients and products, and it is designed with Indian skin tones and climate in mind.
Morning Routine
Step 1: Gentle Cleanse Wash with a pH-balanced, fragrance-free intimate wash. Pat dry gently — do not rub.
Step 2: Apply Brightening Treatment Use a serum or cream containing alpha arbutin (1–2%) and/or niacinamide (4–5%). Apply a small amount and massage gently. Let it absorb for 2–3 minutes.
Step 3: Moisturize Apply a lightweight, fragrance-free moisturizer. Look for glycerin or hyaluronic acid on the label. This step is non-negotiable.
Step 4: Choose Breathable Clothing Wear loose-fitting cotton underwear. Synthetic fabrics trap moisture and create friction — the two biggest enemies of even skin tone in intimate areas.
Evening Routine
Step 1: Cleanse Again (If Needed) A gentle rinse is fine. You do not need to use product every single time.
Step 2: Reapply Moisturizer Keep the area hydrated overnight. Cotton underwear remains important.
Weekly Addition (Once or Twice a Week)
Gentle Exfoliation Use a very mild exfoliant — something with a low concentration of glycolic acid (5–7%) or a gentle enzyme-based scrub. This removes dead skin cells and helps brightening products penetrate better. Never use a physical scrub with harsh beads on this area.
What to Expect
Most people start noticing a subtle change within 4–6 weeks of consistent use. Significant, visible improvement typically takes 6–8 weeks. Everyone’s skin is different, so patience is not optional — it is essential.
Professional Treatment Options (When Home Care Is Not Enough)
If you have been consistent with at-home care for 8–10 weeks and see minimal change, it may be time to explore professional options. In India, these are available at dermatology clinics and aesthetic centres.
Chemical Peels (Superficial) Mild acid peels performed by a dermatologist can remove the top layer of darkened skin and stimulate fresh cell growth. For intimate areas, only superficial peels with very gentle acid concentrations are appropriate. Always ask your doctor about the specific type before agreeing.
Q-Switched Laser Therapy This is one of the most effective professional treatments for intimate hyperpigmentation. The laser targets melanin directly, breaking it down without damaging surrounding tissue. Results are typically visible after 3–5 sessions. It is important to choose a licensed dermatologist or aesthetic clinic — not an unregulated spa.
Microneedling Tiny needles create controlled micro-injuries that stimulate collagen production and regulate melanin activity. It works well for gradual, natural-looking improvement. Results build over 4–6 weeks per session.
Dermamelan Intimate This is a two-phase professional treatment — one in-clinic session followed by at-home gel application for about three months. It is specifically designed for intimate area depigmentation and has shown strong results in clinical settings.
Choosing a Clinic in India — What to Look For
- A board-certified dermatologist or aesthetic gynaecologist
- Clean, professional environment
- Products and lasers approved for use on sensitive skin
- A consultation before any treatment begins (no clinic should skip this)
- Transparent pricing and realistic expectations about timelines
Foods and Lifestyle Habits That Support Skin Brightening
Your skincare routine is only one piece of the puzzle. What you eat, how you dress, and small daily habits all contribute to how your skin responds.
Eat vitamin C-rich foods regularly. Amla (Indian gooseberry), bell peppers, tomatoes, and citrus fruits support melanin regulation from the inside out.
Stay hydrated. Dehydrated skin is more prone to irritation and uneven tone. Aim for at least 2 litres of water a day — more if you exercise regularly.
Reduce friction. Switch to cotton underwear if you have not already. Avoid tight synthetic leggings during workouts. If you shave or wax the bikini area, switch to a gentler hair removal method or use a razor specifically designed for sensitive skin.
Manage stress. Chronic stress increases cortisol, which can influence hormonal balance and skin pigmentation. Even 10 minutes of yoga or meditation can make a difference over time.
Be consistent, not aggressive. The single most important habit for intimate area lightening is showing up every day with a gentle routine — not using the strongest product you can find.
A Quick Personal Note
I have personally dealt with uneven skin tone in my bikini and inner thigh area for years — especially after pregnancy. The products that worked best for me were simple ones: a niacinamide serum used consistently, cotton underwear every single day, and a fragrance-free moisturiser after every wash. It was not glamorous or fast. But after about 6 weeks, the difference was genuinely noticeable. The key lesson? Gentle and consistent always beats harsh and hopeful.
Ingredients to Absolutely Avoid on Intimate Skin
This deserves its own section because the wrong product can do serious, lasting damage.
| Ingredient |
Why It Is Dangerous on Intimate Skin |
| Hydroquinone (above 2%) |
Thins delicate skin; risk of rebound darkening |
| Mercury |
Toxic; banned in many countries but still found in some products |
| Corticosteroids (unsupervised) |
Increases risk of fungal and bacterial infections |
| Strong fragrances or perfumes |
Disrupts natural pH; triggers irritation and inflammation |
| Alcohol (denatured or isopropyl) |
Strips moisture; damages the skin barrier |
| High-concentration glycolic acid (above 10%) |
Too harsh for intimate skin; causes burns |
| Parabens (in sensitive individuals) |
Can trigger allergic reactions on delicate tissue |
Frequently Asked Questions
Q: Is it safe to lighten intimate areas at home? A: Yes, if you use products specifically designed for sensitive skin with gentle, dermatologist-approved ingredients like alpha arbutin, niacinamide, or kojic acid at appropriate concentrations. Always patch test first and avoid anything with harsh chemicals.
Q: How long does it take to see results from intimate area lightening? A: With consistent use of safe, gentle products, most people notice subtle improvement within 4–6 weeks. Significant results typically take 6–8 weeks or longer, depending on skin type and the cause of darkening.
Q: Can I use kojic acid and alpha arbutin together? A: Yes. These two ingredients work through complementary mechanisms — kojic acid blocks copper ions needed for melanin production, while alpha arbutin inhibits the tyrosinase enzyme directly. Together, they can be more effective than either one alone, and both are gentle enough for sensitive skin.
Q: Is hydroquinone safe for intimate area lightening? A: No. Hydroquinone is too harsh for the delicate skin of intimate areas. It can cause skin thinning, irritation, and rebound hyperpigmentation. Safer alternatives like alpha arbutin and kojic acid are strongly preferred.
Q: Why is my intimate area darker than the rest of my body? A: This is completely normal. Skin folds and areas with more friction and hormonal activity naturally produce more melanin. It is not a sign of infection, poor hygiene, or any health problem in most cases.
Q: Can men also lighten intimate areas? A: Absolutely. Men experience darkening in the groin, inner thighs, and underarms just as commonly. The same safe ingredients and gentle routines apply.
Q: Should I see a dermatologist before starting intimate area lightening? A: It is always a good idea, especially if the darkening is sudden, uneven, or accompanied by other symptoms. A dermatologist can rule out any underlying conditions and recommend the best products for your specific skin type.
Q: Does shaving cause intimate area darkening? A: Yes. Shaving creates micro-irritation and inflammation, which stimulates melanin production over time. If possible, switching to a gentler hair removal method or using a high-quality razor designed for sensitive skin can help prevent further darkening.
Final Conclusion
Darkening in intimate areas is one of the most common skin concerns — yet one of the least openly discussed. The good news is that safe, effective intimate area lightening safe methods exist, and they do not require harsh chemicals, expensive clinic visits, or risky home experiments.
The foundation of any good approach is gentleness: the right ingredients at the right concentrations, consistent daily use, proper hydration, and breathable clothing. Alpha arbutin, niacinamide, and kojic acid are your best allies here — all backed by solid dermatological research and gentle enough for even the most sensitive skin.
If you take just one thing away from this article, let it be this: slow and steady genuinely wins this race. Your intimate skin deserves the same care, patience, and respect you give to the rest of your body. Start gentle, stay consistent, and the results will follow.